How Anti-Microbial Resistance could happen so quickly
Today is the last day of the World Health Organization’s Antimicrobial Awareness Week.
Antibiotics have been used to treat sick people for no more than 80 years. Most of us know people who were around in the pre-antibiotics era! Thinking about that does make one wonder about how an evolutionary process such as antibiotic resistance could happen so (relatively) quickly.
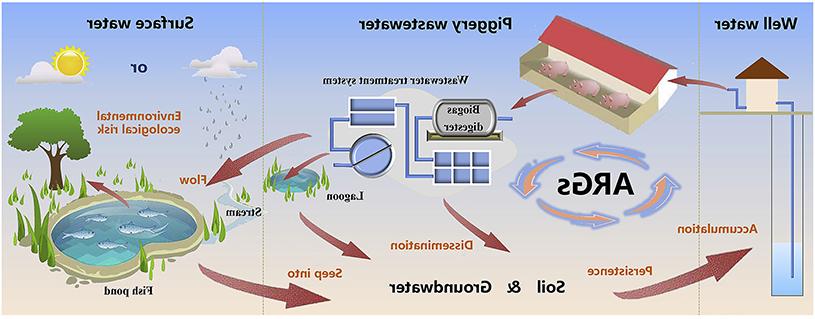
The resistant bacteria, fungi or viruses are commonly found in people, animals, food, plants and the environment (water, soil and air). They can be spread from person to person, from people to animals, and from food to humans or animals. The links between these sources are tight, and this is the main reason that we should consider all fractions as one, and we should take measures that cover them all.
Anti-Microbial Resistance: natural evolution
Normally Anti-Microbial Resistance (AMR) occurs over time because of genetic changes within microorganisms. This process is natural to evolution. However the misuse of antibiotics in human and animal health has caused this process to speed up immensely. Other agricultural and livestock practices may also have contributed to the emergence of one of the biggest threats of our modern human history.
The development and transference of Antibiotic Resistance Genes (ARG’s)
Bacteria that are constantly exposed to incorrect levels of antimicrobials, eventually develop Antibiotic Resistance Genes (ARG). These genes can then migrate from farming waste to soil, from soil to water, from water to crop and into the population.
Antibiotic Resistance Genes may be picked up by other microorganisms, and these organisms can also learn how to be resistant to specific antimicrobials, even if they have never been exposed to them before. This may be one of the explanations why only in 8 decades we have reached such a high level of resistance. This cycle is an infinite process, that can only be stopped by effectively managing the usage of antibiotics on a global scale.
A global issue with legislation as an answer
Research shows that chronic overuse or misuse of antibiotics is more prevalent in low to mid income regions. Legislations with the objective of responsibly limiting the use of antimicrobials are often not in place there.
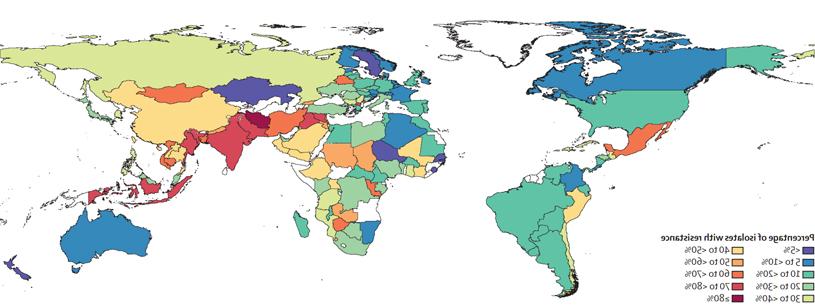
The above map represents the percentage of third generation cephalosporin resistant E. coli found in samples gathered by the University of Washington. On average farm animals harbor more drug resistant bacteria in countries where meat production has increased rapidly. Source: http://www.thelancet.com/action/showPdf?pii=S0140-6736%2821%2902724-0
Are antibiotics “the bad guy”?
In order to decrease or even stop the propagation of these ARG’s originating from agricultural industries, it is important to understand the need for good management practices and the implementation of HACCP rules in farms and feed mills. This does not mean that we should give up on antibiotics. For curative purposes we often don’t have any other tools at our disposal. That is why understanding AMR, expanding our knowledge of antibiotics and their correct usage, and closely monitoring administration of application are needed to prevent further rise of resistant genes.
Holistic approaches that involve feed hygiene, feed or water acidification and promoting gut health are proven tools to mitigate pathogens and their effects. The classic motto ‘prevention is better than curing’ holds true to this day. Contact one of our experts or your sales manager if you would like to discuss this topic in more detail.
 Source:
Source: